New SRMC lab equipment speeding up diagnoses
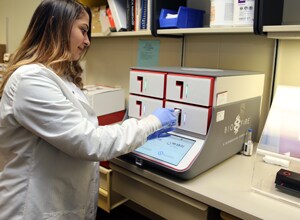
A new piece of equipment at Southeastern Regional Medical Center will significantly shorten wait times for a variety of tests. The BioFire Film Array Torch System will help clinicians make vital decisions regarding admission, isolation, antiviral or antibiotic therapy, and additional diagnostic testing. In a revolutionary change for laboratory testing process, tests that previously took multiple hours, or even days to complete, can now be performed in a little over an hour in the analyzer.
The BioFire can run five different panels: blood culture identification, gastrointestinal, meningitis/encephalitis, pneumonia and respiratory. Each panel focuses on separate types of symptoms to narrow down the specific pathogen, whether virus, bacteria or parasite, causing the symptoms, as well as several antibiotic-resistant strains. The machine allows physicians to quickly target the correct pathogen with the correct treatment, which also improves the hospital’s antimicrobial stewardship. Pathologist Dr. Ricky Johnson, the medical director for SRMC Laboratory Services, said that while the analyzer will initially be used for hospital patients only, when all the panels are rolled out, certain outpatient specimens will also be accepted. Patients at other clinics or labs can simply request that their test be sent to the SRMC lab.
The first panel that will be implemented at SRMC will be the blood culture identification (BCID) panel, which is expected to go live by the end of February. The BCID panel includes 27 of the most common causes of bloodstream infections, such as different strains of streptococcus, different strains of the bacteria family that includes E.coli and salmonella, and yeast. The BCID will also be able to determine the presence of the antimicrobial resistance genes methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococci (VRE), and carbapenem-resistant Enterobacteriaceae (CRE). This is important because it will allow clinicians and pharmacists to isolate and treat patients faster than previous methods have allowed.
“The BioFire will rapidly reduce the time to identification, allowing for timely and optimal patient treatment and satisfaction,” said SRMC Microbiology Supervisor Erin Hunt. “The BioFire will also allow us to reduce turn-around time for bacteria identification. Traditional culture methods can take up to 48 hours or longer to identify a pathogen. The BioFire will be able to identify pathogens directly from a patient’s specimen. This analyzer uses polymerase chain reaction (PCR) technology to detect the DNA of a virus, bacteria or parasite. It’s more versatile, faster, easy to use, and highly specific and sensitive. Antibiotic stewardship, together with the BCID panel, will allow for shortened time to optimal therapy, decreased unnecessary antibiotic use, and decreased time to antimicrobial de-escalation.”
From a patient’s perspective, the time saved with this equipment might be the difference between staying at the hospital overnight for observation or being sent home the same day with the most effective prescription. It also cuts down on the amount of blanket antibiotics that patients will receive while doctor’s wait for test results, which is an important part of the global effort to slowing the growth of drug-resistant microbes.
The BioFire also decreases the number of send-out tests and allows the lab to do more tests in-house. Several tests, such as norovirus, whooping cough, and walking pneumonia, are currently sent off-site and may take days or weeks for results to return.